Winter 2023 (Volume 33, Number 4)
Celebrating 50 Years of HLA-B27 and Axial Spondyloarthritis:
Top 10 Common Questions Answered
By Ibraheem Almani, MD; and
Akihiro Nakamura, MD, PhD
Download PDF
1. What is HLA-B27? What role does HLA-B27 play?
The human leukocyte antigen B27 (HLA-B27), a unique label on the surface of our cells, plays a pivotal role in the immune system. This antigen helps our immune system by showing off pieces (peptides) of pathogenic antigens (like viruses and dying cells) to other immune cells called cytotoxic T cells. When the cytotoxic T cells receive the signal, they swoop in and get rid of the troublemakers, thereby contributing to immune surveillance and response.1
2. Which diseases are linked to HLA-B27?
The most striking association is with axial spondyloarthritis (axSpA), where up to 90% of ankylosing spondylitis (AS) and around 70-80% of non-radiographic
axSpA patients possess the HLA-B27 allele, respectively.2,3 Besides axSpA, HLA-B27 is also associated with other diseases within the SpA spectrum, such as acute anterior uveitis, psoriatic arthritis, reactive arthritis, and juvenile idiopathic arthritis.4-7 Furthermore, there have been reports of an association between inflammatory bowel diseases (IBD) such as Crohn's disease and ulcerative colitis and HLA-B27, although conclusive evidence has yet to be established.8
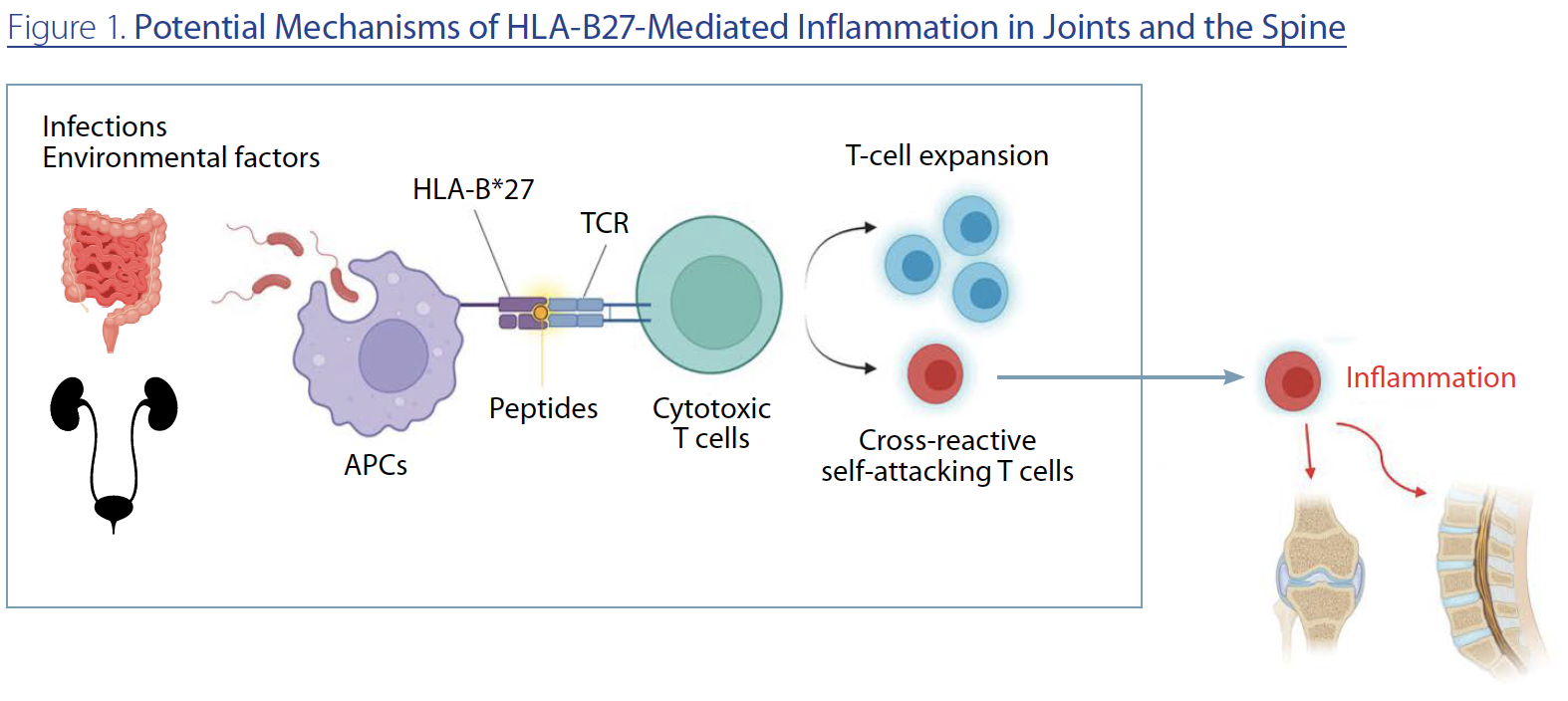
3. How does HLA-B27 cause these diseases?
The short answer is that we don’t know yet. However, HLA-B27, in combination with other genetic variants, is thought to lead to the chronic activation of downstream immune cells.9,10 This activation might be mediated by an abnormal gut microbiome, in which HLA-B27 presents disease-associated peptides to downstream T cells. Subsequently, cross-reactive self-attacking T cells migrate to the joints and spine, causing inflammation (Figure 1). It’s worth noting that up to 60% of axSpA patients exhibit clinical or subclinical inflammation in the gut.11 Furthermore, HLA-B27 transgenic mice do not develop SpA symptoms under germ-free conditions.12 These facts demonstrate a close relationship between the gut and
axSpA, and also suggest that specific peptides presented by HLA-B27 in the gut activate downstream T-cell responses leading to SpA-spectrum diseases.
4. Does the HLA-B27 test need to be repeated?
Once a patient has tested positive or negative for HLA-B27 based on established methods such as PCR, the test does not need to be repeated as the presence of this antigen is a stable trait that does not change over time.13
5. What is the prevalence of HLA-B27 in the general population?
The prevalence of HLA-B27 in the general population varies significantly across different ethnic groups and geographic regions. On a global average, approximately 6-8% of individuals carry the HLA-B27 antigen, and the Canadian population frequency is also reported to be around 7%. Notably, the prevalence is as low as less than 1% in the Japanese population, to as high as approximately 24% in certain indigenous populations of Alaska.14-16
6. If someone is HLA-B27 positive, what is their likelihood of developing axSpA?
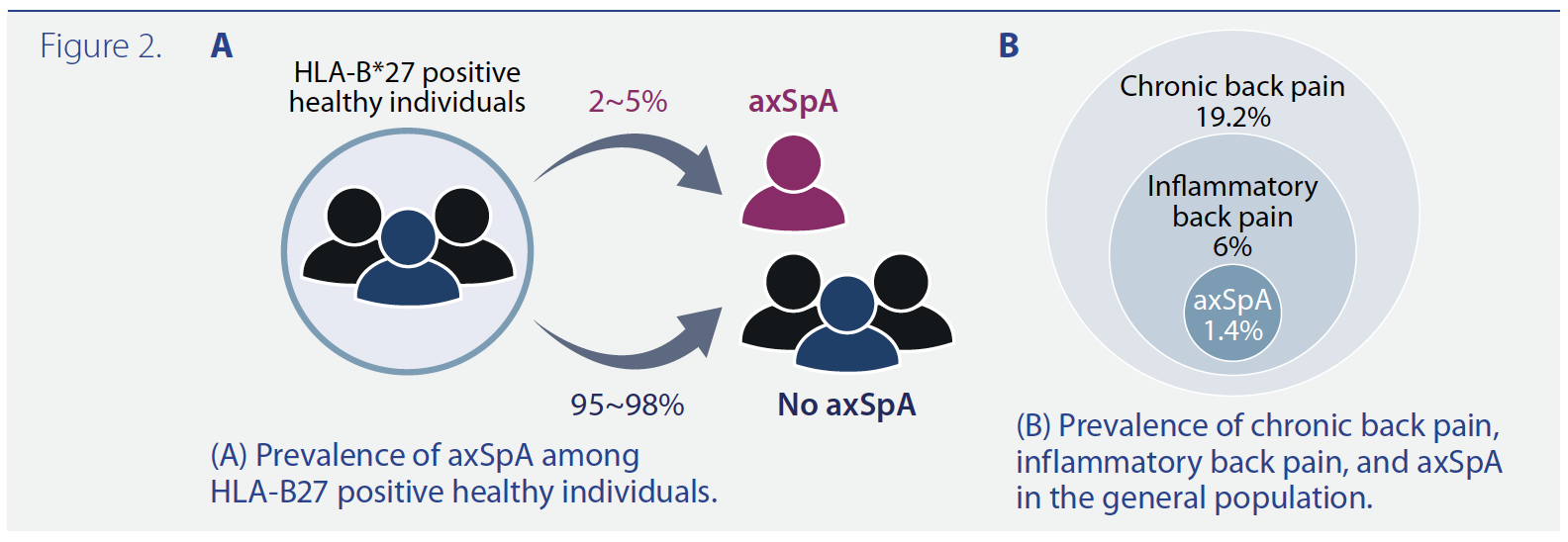
It is known that HLA-B27-positive individuals face a lifetime risk of approximately 2-5% for the development of axSpA (Figure 2A), compared to around 1% in the general population.17 While this risk is higher than that in the general population, it’s important to note that more than 95% of HLA-B27-positive individuals do not develop axSpA.
However, the risk is higher for individuals who not only carry the HLA-B27 antigen but also have a first-degree relative with axSpA, with estimates at around 20%.18
7. Are genetic tests necessary for other family members if one tests positive for HLA-B27?
Despite the hereditary component associated with HLA-B27, genetic testing for HLA-B27 status in asymptomatic family members is not typically recommended or required. Testing is usually reserved for those presenting with suggestive clinical symptoms of an HLA-B27-associated condition.
8. Is it recommended for HLA-B27-positive individuals to consult rheumatologists?
While HLA-B27 alone without any symptoms does not require a rheumatology consultation, when an individual tests positive for HLA-B27 and is experiencing symptoms indicative of a rheumatic condition, it is recommended to consult a rheumatologist for a comprehensive assessment. It is also important to note that although around 20% of the general population has chronic back pain, with 6% being inflammatory back pain, only 1.4% of them have axSpA (Figure 2B).19
9. What does a positive HLA-B27 result signify in patients with axSpA?
In the context of axSpA, HLA-B27 positivity is known to be a risk factor for earlier disease onset, a more severe disease course, the development of new bone formation, and a higher incidence of extra-articular manifestations such as anterior uveitis.20
10. Does the presence of HLA-B27 affect the response to treatment or the prognosis of axSpA?
Data on the correlation between HLA-B27 status and treatment response in axSpA are diverse and somewhat ambiguous. However, previous studies have reported a better response in HLA-B27-positive patients toward tumor necrosis factor inhibitors (TNFi).21-24 Regarding prognosis, while axSpA disease may impact life expectancy compared to general populations, carrying HLA-B27 variants itself does not increase mortality risks in either axSpA patients or healthy individuals.25
Acknowledgment: Figure 1 and Figure 2 were created with BioRender (BioRender.com).
Ibraheem Almani, MD
Rheumatology Fellow, Department of Medicine,
Division of Rheumatology,
Queen’s University, Kingston, Ontario
Akihiro Nakamura, MD, PhD
Assistant Professor, Department of Medicine
Division of Rheumatology, Queen’s University
Clinician Scientist, Translational Institute of Medicine, School of Medicine,
Department of Medicine, Queen’s University,
Kingston, Ontario
Suggested readings:
1. Ranganathan V, Gracey E, Brown MA, et al. Pathogenesis of ankylosing spondylitis - recent advances and future directions. Nat Rev Rheumatol. 2017 Jun; 13(6):359-367. PMID: 28446810.
2. Nakamura A, Boroojeni SF, Haroon N. Aberrant antigen processing and presentation: Key pathogenic factors leading to immune activation in Ankylosing spondylitis. Semin Immunopathol. 2021 Apr; 43(2):245-253. PMID:33532928.
3. Yang X, Garner LI, Zvyagin IV, et al. Autoimmunity-associated T cell receptors recognize HLA-B*27-bound peptides. Nature. 2022; 612:771–7. PMID: 36477533.
References:
1. Bowness P. HLA-B27. Annu Rev Immunol. 2015;33:29-48. doi: 10.1146/annurev-immunol-032414-112110. PMID: 25861975.
2. Hwang MC, Ridley L, Reveille JD. Ankylosing spondylitis risk factors: a systematic literature review. Clin Rheumatol. 2021 Aug;40(8):3079-3093. doi: 10.1007/s10067-021-05679-7. Epub 2021 Mar 22. PMID: 33754220.
3. Zhang S, Wang Y, Peng L, et al. Comparison of Clinical Features in HLA-B27 Positive and Negative Patients With Axial Spondyloarthritis: Results From a Cohort of 4,131 Patients. Front Med (Lausanne). 2020 Dec 23;7:609562. doi: 10.3389/fmed.2020.609562. PMID: 33425955.
4. Chatzikyriakidou A, Voulgari PV, Drosos AA. What is the role of HLA-B27 in spondyloarthropathies? Autoimmun Rev. 2011 Jun;10(8):464-8. doi: 10.1016/j.autrev.2011.01.011. Epub 2011 Feb 4. PMID: 21296192.
5. Duba AS, Mathew SD. The Seronegative Spondyloarthropathies. Prim Care. 2018 Jun;45(2):271-287. doi: 10.1016/j.pop.2018.02.005. PMID: 29759124.
6. Kavadichanda CG, Seth G, Kumar G, et al. Clinical correlates of HLA-B*27 and its subtypes in enthesitis-related arthritis variant of juvenile idiopathic arthritis in south Indian Tamil patients. Int J Rheum Dis. 2019 Jul;22(7):1289-1296. doi: 10.1111/1756-185X.13551. Epub 2019 Mar 18. PMID: 30884197.
7. D'Ambrosio EM, La Cava M, Tortorella P, et al. Clinical Features and Complications of the HLA-B27-associated Acute Anterior Uveitis: A Metanalysis. Semin Ophthalmol. 2017;32(6):689-701. doi: 10.3109/08820538.2016.1170158. Epub 2016 Jul 12. PMID: 27404944.
8. Parameswaran P, Lucke M. HLA-B27 Syndromes. 2023 Jul 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 31855367.
9. Nakamura A, Boroojeni SF, Haroon N. Aberrant antigen processing and presentation: Key pathogenic factors leading to immune activation in Ankylosing spondylitis. Semin Immunopathol. 2021 Apr;43(2):245-253. PMID:33532928.
10. Ranganathan V, Gracey E, Brown MA, et al. Pathogenesis of ankylosing spondylitis - recent advances and future directions. Nat Rev Rheumatol. 2017 Jun;13(6):359-367. PMID: 28446810
11. Mielants H, Veys EM, Cuvelier C, et al. The evolution of spondyloarthropathies in relation to gut histology. III. Relation between gut and joint. J Rheumatol. 1995 Dec;22(12):2279-84. PMID: 8835562
12. Taurog JD, Richardson JA, Croft JT, et al. The germfree state prevents development of gut and joint inflammatory disease in HLA-B27 transgenic rats. J Exp Med.1994 Dec 1;180(6):2359-64. PMID: 7964509
13. Suresh E. Laboratory tests in rheumatology: A rational approach. Cleve Clin J Med. 2019 Mar;86(3):198-210. doi: 10.3949/ccjm.86a.18076. PMID: 30849037.
14. Khan MA. Epidemiology of HLA-B27 and Arthritis. Clin Rheumatol. 1996 Jan;15 Suppl 1:10-2. doi: 10.1007/BF03342637. PMID: 8835494.
15. Sheehan NJ. The ramifications of HLA-B27. J R Soc Med. 2004 Jan;97(1):10-4. doi: 10.1177/014107680409700102. PMID: 14702356.
16. Ziade NR. HLA B27 antigen in Middle Eastern and Arab countries: systematic review of the strength of association with axial spondyloarthritis and methodological gaps. BMC Musculoskelet Disord. 2017 Jun 29;18(1):280. doi: 10.1186/s12891-017-1639-5. PMID: 28662723.
17. Brown MA, Xu H, Li Z. Genetics and the axial spondyloarthritis spectrum. Rheumatology (Oxford). 2020 Oct 1;59(Suppl4):iv58-iv66. doi: 10.1093/rheumatology/keaa464. PMID: 33053195.
18. van der Linden SM, Khan MA, Li Z, Baumberger H, et al. Factors predicting axial spondyloarthritis among first-degree relatives of probands with ankylosing spondylitis: a family study spanning 35 years. Ann Rheum Dis. 2022 Jun;81(6):831-837. doi: 10.1136/annrheumdis-2021-222083. Epub 2022 Mar 11. PMID: 35277388.
19. Reveille JD, Witter JP, Weisman MH. Prevalence of axial spondylarthritis in the United States: estimates from a cross-sectional survey. Arthritis Care Res (Hoboken). 2012 Jun;64(6):905-10. doi: 10.1002/acr.21621. PMID: 22275150.
20. Akkoç N, Yarkan H, Kenar G, et al. Ankylosing Spondylitis: HLA-B*27-Positive Versus HLA-B*27-Negative Disease. Curr Rheumatol Rep. 2017 May;19(5):26. doi: 10.1007/s11926-017-0654-8. PMID: 28386763.
21. Arends S, van der Veer E, Kallenberg CG, et al. Baseline predictors of response to TNF-α blocking therapy in ankylosing spondylitis. Curr Opin Rheumatol. 2012 May;24(3):290-8. doi: 10.1097/BOR.0b013e32835257c5. PMID: 22418743.
22. Arends S, Brouwer E, van der Veer E, et al. Baseline predictors of response and discontinuation of tumor necrosis factor-alpha blocking therapy in ankylosing spondylitis: a prospective longitudinal observational cohort study. Arthritis Res Ther. 2011 Jun 20;13(3):R94. doi: 10.1186/ar3369. PMID: 21689401.
23. Vastesaeger N, van der Heijde D, Inman RD, et al. Predicting the outcome of ankylosing spondylitis therapy. Ann Rheum Dis. 2011 Jun;70(6):973-81. PMID: 21402563.
24. Fröhlich F, Micheroli R, Hebeisen M, et al. HLA-B27 as a predictor of effectiveness of treatment with TNF inhibitors in axial spondyloarthritis: data from the Swiss Clinical Quality Management Registry. Clin Rheumatol. 2023 May;42(5):1267-1274. PMID: 36574181.
25. Li Z, Khan MK, van der Linden SM, et al. HLA-B27, axial spondyloarthritis and survival. Ann Rheum Dis. 2023 Sep 7;ard-2023-224434. PMID: 37679034.
|
