Spring 2020 (Volume 30, Number 1)
Transition to a Successful Retirement:
A Personal Perspective
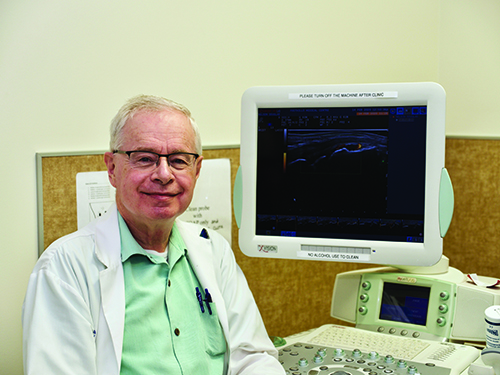
By Christopher Penney, MD, FRCPC
Download PDF
The transition from a busy medical practice to retirement can be done in many ways and is subject to personal circumstances, planning or lack thereof, and just plain luck. I have been fortunate to be able to plan a slow exit over the past three years. This slow exit has benefited both me and my patients.
To put things into context, after completing rheumatology training in London Ontario, I began private practice rheumatology in Calgary in 1982. In 2004, after receipt of an
Arthritis Society Clinician-Teacher Award, I became a salaried clinician teacher at the University of Calgary. My passions have been bedside teaching, physical examination, photography at divisional events, and, for the past eight years, point-of-care musculoskeletal (MSK) ultrasound. My colleagues and I have kindled local interest in rheumatology to the point where there are now nearly enough rheumatologists in Southern Alberta.
I am in the third year of my transition to full retirement. A little more than two years ago, I resigned from my salaried position at the University of Calgary and transferred the care of all my patients to my colleagues. I was fortunate that the university hired Dr. Stephen Thomson, a young clinician teacher, to replace me and take over my teaching duties and many of my patients. Because my retirement was planned, I was able to give all my patients a big hug on their last visit and wish them the best. Drs. Stephen Thomson and Caylib Durand are taking over as the divisional event photographers.
There is a constant weight and strain to medical practice. Despite advances in therapeutics, most of our chronic systemic inflammatory patients become what in Chinese cooking are known as “pot stickers,” and are with us for our practice lifetime. With my retirement from full-time practice came a sense of freedom.
What have I been doing in semi-retirment? For the first two years, I ran a triage clnic where I saw low-priority, mainly chronic soft-tissue pain patients. Those patients would otherwise have to wait six to 12 months. At least in Calgary,
our resources have been mainly directed at inflammatory
diseases, and these patients have been largely ignored. I do a point-of-care ultrasound clinic for my colleagues, and bang the drum for the usefulness of ultrasound in routine rheumatology practice. Because I have more free time, I am now able to exercise more and take better care of my own health. Betty, my dear wife, became quite ill one year ago, and I have been able to attend her doctors’ appointments and help her.
This year, my plan is to do an MSK ultrasound clinic once a week, do as-needed temporal artery ultrasound exams, and help with ultrasound research projects. I have just pitched in to do some clinics for a colleague who is off for eight weeks on sick leave. I will also continue to do some physical examination teaching.
I would like to thank the University of Calgary for allowing my phased retirement. In particular, I thank Drs. Dianne Mosher and Paul MacMullan, the past and current Division of Rheumatology directors. Also special thanks to Dr. Susan Barr for her help and encouragement over the past eight years as we have both learned and are still learning to do point-of-care ultrasound.
Christopher Penney, MD, FRCPC
Rheumatologist,
Calgary, Alberta
|
