Fall 2014 (Volume 24, Number 3)
Analysis of Rheumatology Nursing Interventions in Out-patient Practice Settings
By Muxin Sun, MD;
Shahin Jamal, MD, FRCPC, MSc; and
Jason Kur, MD, FRCPC
Download PDF
Objectives: To describe the characteristics of patients referred for nursing assessments in rheumatologist offices and types of interventions performed.
Methods: The electronic charts of patients seen by a rheumatology nurse between January and March 2012 in three Vancouver-based rheumatologists’ offices were reviewed.
Results: Data was extracted on 300 patients. The most common disease referral was rheumatoid arthritis (RA), followed by connective tissue disease, ankylosing spondylitis (AS), psoriatic arthritis (PsA), and other diagnoses. In total, 895 interventions were performed. Rheumatic disease counselling, disease-modifying anti-rheumatic drug (DMARD) counselling, and general education were implemented in 277 patients. Methotrexate (MTX) and biologic subcutaneous administration and/or education were given to 81 patients. Tuberculosis (TB) skin test and immunizations were also performed on 11 and 127 patients, respectively.
Conclusion: Education was the most common service offered to patients referred for nursing assessment, along with immunizations and TB skin tests. Addition of rheumatology nurses provides services that are key elements of management for patients with rheumatic diseases.
Introduction
Rheumatic diseases hinder many aspects of a patient’s life, making them highly reliant on the medical system.1 Management of chronic rheumatic diseases now requires a multidisciplinary effort with a spectrum of health care providers and complex treatment strategies.2-7 Most require lifelong management plans, aiming to induce remission, suppress disease activity, maintain function, and develop coping strategies.1,8 With the advent of intravenous (IV) and subcutaneous (SC) biologics, rheumatic patients have seen enormous advancements in their disease control.9,10 Healthcare models must be adapted to teach proper and safe administration of these newer therapies to a wide population, including the elderly or those with impaired joint mobility.
In the United States and Europe, nurses are comprehensively integrated into rheumatology clinics.11 This model can increase the efficiency of rheumatology clinics, curtailing long wait times due to rheumatologist shortages and improving patient care.2,12 This is especially relevant as the current management of inflammatory diseases emphasizes rapid access to specialized care to receive early targeted treatment before joint damage develops.13
Nursing care has been shown to have a long-term positive impact in multiple disease-related psychosocial issues, such as depression, pain, and fatigue, major features in many RA patients.2,8,11,14-17 Satisfaction with care translates to improved patient compliance with treatment, functional ability, and well-being in chronic diseases.18,19 Additionally, having a nurse present to provide active education and support may help avoid unnecessary consultations with the general practitioner.11 Many of the services offered by nurses with training in rheumatology are recommended interventions by the American College of Rheumatology (ACR), British Society for Rheumatology (BSR), and European League Against Rheumatism (EULAR) in the management of rheumatic diseases.13,20,21 These include vaccinations, monitoring for drug side effects, and TB screening. Similarly, the BSR and EULAR guidelines for RA emphasize the importance and benefit of rheumatology nursing support.4,21 Overall, the most successful outcome for patients is achieved when the skills of physicians and nurses are combined, utilizing their expertise appropriately and in a time-efficient manner.14
Currently, nursing support is well established in a number of fields including diabetes, heart failure, and psychiatric care. This study will examine the scope of interventions and education performed by nurses in outpatient rheumatology practice settings following funding for access to this added service.
Materials and Methods
Patients were identified by use of a new billing code indicating that they were seen in conjunction with a rheumatology nurse. The electronic charts of all patients who had a visit labelled as “31060” between
January 1, 2012 and March 31, 2012 in three different Vancouver-based, outpatient rheumatology offices were reviewed. Patients underwent medical review with the rheumatologist first and, if deemed appropriate, were then referred to the clinic nurse for multi-disciplinary care needs. Interventions performed by the nurse were recorded in the electronic medical record (EMR). Each of the three clinics had one nurse per rheumatologist. These registered nurses have received supplemental training in rheumatology though local and national courses, as well as observerships in rheumatology practices. The goals of their training were based on professional nursing competencies set out by the ACR.
The inclusion criteria for the 31060 code are: patient must be seen by a rheumatologist; only to be used for the ongoing management of complex disorders of the musculoskeletal system, where the complexity of the condition requires continuing management by a rheumatologist, and not to be used for uncomplicated rheumatologic disorders; patient must be seen by a registered nurse; and use once per patient every six months.
Patient variables included: date of visit, sex, age, and rheumatologic diagnosis. Disease duration and activity parameters, co-morbidities, and medications were not included. Rheumatologic diagnosis was identified using the International Classification of Diseases (ICD-9) code.
Data was extracted by the individual nurse from each office through retrospective chart review. Each intervention was recorded based on available documentation within the EMR. Data collection was not corroborated by a second extractor.
The nursing interventions for each patient visit were categorized and recorded as dichotomous variables (done/not done). There was no limit to the number of interventions per visit. Interventions performed up to two weeks before or after the nursing visit were permitted for inclusion
(e.g., reading a TB skin test). Nursing interventions included:
1. Education about IV biologic therapy for a first start;
2. Administration of an IV biologic;
3. Education about SC biologic therapy for first start;
4. Administration of a SC biologic;
5. Teaching patient to self-administer SC MTX for a first start;
6. Administration of SC MTX;
7. Rheumatic disease education;
8. General education regarding lifestyle modification, nutrition, weight loss strategies, pain control, dental hygiene, family planning, joint protection;
9. DMARD counselling including hydroxychloroquine, oral MTX, sulfasalazine, leflunomide, azathioprine, and mycophenolate mofetil;
10. Performing and reading the TB skin test;
11.General advice on immunizations and/or administration of influenza/pneumococcal vaccine;
12. Other interventions: an open field for additional nursing services performed that were not listed above.
Descriptive statistics were used to calculate the frequency of each individual intervention as well as the different combinations of interventions performed.
Results
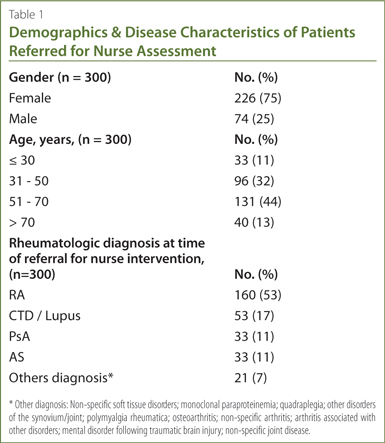
Data from 300 patients were collected from the three consultant rheumatologist offices. Demographic information is summarized in
Table 1. The female to male ratio was approximately 3:1. The majority of patients were between the ages of 50 to 70, but the youngest and oldest patient to receive nursing assessment were 21 and 88 years old, respectively.
This patient sample had a total of 18 different diagnoses based on their identified ICD-9 code on referral to the nurse. The most commonly referred rheumatologic diagnosis was RA, followed by connective tissue disease (CTD)/lupus, AS, and PsA. Other diagnoses were less likely to be referred for nursing assessment (Table 1).
In total, registered nurses performed 895 interventions on the 300 patients reviewed. Table 2 lists the type as well as the number of times an intervention was recorded as being performed. The most frequent nursing interventions were general education, rheumatic disease counselling, and other interventions. In the “other interventions” category, various other duties were performed, with the most common being physician supervised drug monitoring performed on 97 patients. This was followed by a teaching review of DMARDs or biologics for patients already on therapy.
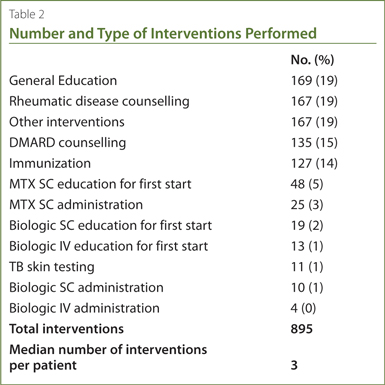
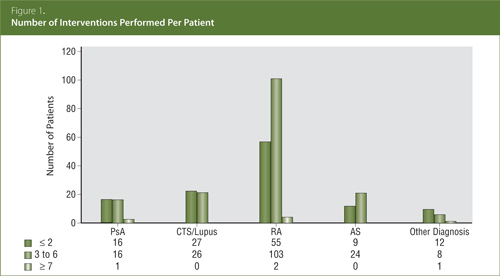
The majority of patients had more than one intervention per visit; the highest incidence was three interventions (91 patients), followed by two interventions (78 patients), and four interventions (47 patients). The greatest number of interventions on a single visit was 10. The median number of interventions per patient was three, and was consistent across all diagnoses. Figure 1 shows the breakdown of the number of interventions per patient in accordance to their diagnosis.
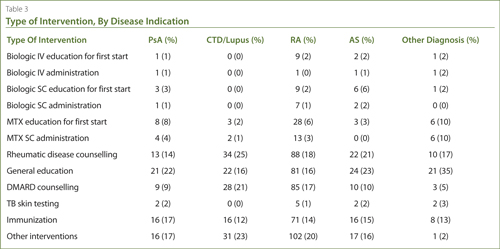
Comparing the type of intervention to rheumatologic diagnosis (Table 3), there was a similar pattern of distribution across all diseases. Rheumatic disease counselling, DMARD counselling, and general education were the most often performed. The number of patients who received at least one of the above services included 29 PsA patients, 51 CTD/Lupus patients, 145 RA patients, 31 AS patients, and 21 patients with other diagnoses, for a total of 277 of 300 patients. MTX and biologic administration and/or education were given to 81 patients in this review. TB skin testing and immunization were also performed on 11 and 127 out of the 300 patients, respectively.
Discussion
Our data indicates that patient education is a large component of services offered by nurses to rheumatology patients. This not only includes disease specific counselling and medication teaching, but also a substantial amount of non-pharmacologic education (e.g., joint protection techniques, family planning), which are widely reported as being of therapeutic value.4,5 BSR and EULAR also recommend education be offered to every patient with inflammatory arthritis.4,21 Dedicated patient teaching and nursing consultation has been demonstrated to improve patient behaviours,6 increase understanding about adverse drug reactions,7,22 and results in better patient compliance.23 Given improved adherence, patients may have better control of their disease, potentially decreasing the economic burden of illness; patient education is thus an integral part of the successful management of rheumatologic diseases.23 More importantly, those who require SC MTX or biologics have more severe disease, and early education with optimal adherence has been shown to reduce long-term disability and hospitalizations.1,24
Other interventions, including drug monitoring, were performed 167 times, suggesting that there are many other nursing activities that may have added benefits beyond the pre-set options in this review. Physician-supervised medication monitoring was widely performed by nurses, potentially decreasing emergency department visits due to medication complications or disease flares.
The ACR recommends regular drug monitoring for side effects, as well as TB skin tests and scheduled vaccinations for patients with RA13 in addition to SC and IV therapies. In our current medical system, patients require multiple visits to receive multifaceted medical care
(e.g., counselling, diagnostic testing, and complex medication injections). In this review, over 92% of patients (277/300) received education (regarding rheumatic diseases, DMARD counselling, non-pharmacologic therapies, or a combination of all three), 11 received TB skin tests, 127 were given immunizations, and 81 underwent non-oral immunosuppressant education and administration (related to MTX and/or biologics). Thus, without direct access to multidisciplinary nursing care, these patients would have required a combined total of 496 visits to other health care providers compared to the 300 nursing visits provided. This is an almost 40% decrease. With a single point-of-care at the office, these services can be offered in one setting, thereby helping reduce demand on the health care resources of British Columbia. A previous study also reflected these findings, with the number of doctor visits decreasing by 35% over 20 months of follow up after patient educational sessions.25 Streamlining visits in this manner can lead to a significant reduction in health care costs.
Incorporating nursing management for rheumatologic diseases can provide rheumatologists with more time to concentrate on problematic cases or new consults, while nurses supply much needed support in teaching SC injections, TB skin tests, and vaccinations.14 Studies demonstrate that lack of access to rheumatology services has been associated with the underuse of DMARDs and an increase in acute flares and hospitalizations.26
Our study has several limitations. First, we do not know the amount of time spent by the nurse with each patient. We estimate that, given such extensive education requirements in rheumatic diseases, a minimum of 30 minutes would be spent per patient; this may, however, be an underestimation in that some patients received multiple interventions. Moreover, the field of rheumatologic nursing is relatively new, with nursing roles still evolving. There are no set educational guidelines dictating outpatient rheumatology nursing practice and different nurses may vary in their delivery of patient education.
Our patient data were identified through billing codes; however, we were unable to capture data on patients who saw a nurse without a corresponding code due to billing restrictions. It is likely there were other patients seen by the rheumatology nurse where the intervention data was not captured.
Lastly, in this analysis, no disease outcome data was collected, nor did we assess patient and physician satisfaction or patient outcomes with nursing interventions. We cannot specifically quantify whether there was a change in healthcare utilization or a decrease in other healthcare visits after implementation of nursing care, as this was not measured. Comparing rates of non-adherence and complications between a nurse-involved group and a control group would be useful. As these nursing visits are a single encounter, longer-term studies with review of periodic nursing involvement and the effect on clinical outcomes would be constructive.
This study has demonstrated that a wide variety of nursing interventions were provided after the implementation of a multidisciplinary rheumatology nursing code. These assessments can provide many recommended essential therapies for rheumatic patients. We believe these services have the potential to improve comprehensive patient care, increase rheumatologist clinic efficiency, and reduce visits to other health care professionals.
We are grateful to Dr. Kam Shojania who, in addition to the clinical authors, entered patients into the review. We are also grateful to Bonnie Leung, Patricia Patrick, and Sheryl Rosenhek, the rheumatology registered nurses involved in the data collection. Finally we are grateful for the statistical advice of Dr. Kerry Wilbur, of Qatar University.
References
1. Kvien TK. Epidemiology and burden of illness of rheumatoid arthritis. Pharmacoeconomics 2004; 22(2 Suppl 1):1-12.
2. Ryan S, Hassell AB, Lewis M, et al. Impact of a rheumatology expert nurse on the wellbeing of patients attending a drug monitoring clinic. J Adv Nurs 2006; 53(3):277-86.
3. Tijhuis GJ, Zwinderman AH, Hazes JM, et al. Two-year follow-up of a randomized controlled trial of a clinical nurse specialist intervention, inpatient, and day patient team care in rheumatoid arthritis. J Adv Nurs 2003; 41(1):34-43.
4. Vliet Vlieland TP, Pattison D. Non-drug therapies in early rheumatoid arthritis. Best Pract Res Clin Rheumatol 2009; 23(1):103-16.
5. Tucker M, Kirwan JR. Does patient education in rheumatoid arthritis have therapeutic potential? Ann Rheum Dis 1991; 50 Suppl 3:422-8.
6. Brus HL, van de Laar MA, Taal E, et al. Effects of patient education on compliance with basic treatment regimens and health in recent onset active rheumatoid arthritis. Ann Rheum Dis 1998;57(3):146-51.
7. Kirwan JR. Patient education in rheumatoid arthritis. Curr Opin Rheumatol 1990; 2(2):336-9.
8. Hill J, Thorpe R, Bird H. Outcomes for patients with RA: a rheumatology nurse practitioner clinic compared to standard outpatient care. Musculoskeletal Care 2003; 1(1):5-20.
9. Singh JA, Christensen R, Wells GA, et al. A network meta-analysis of randomize controlled trials of biologics for rheumatoid arthritis: a Cochrane overview. CMAJ 2009; 181(11):787-96.
10. Agarwal SK. Biologic agents in rheumatoid arthritis: an update for managed care professionals. J Manag Care Pharm 2011; 17(9 Suppl B):S14-8.
11. van Eijk-Hustings Y, van Tubergen A, Boström C, et al. EULAR recommendations for the role of the nurse in the management of chronic inflammatory arthritis. Ann Rheum Dis 2012; 71(1):13-9.
12. Kur J, Koehler B. Rheumatology demographics in British Columbia; A looming crisis. BCMJ 2011; 53(3):128-31.
13. Singh JA, Furst DE, Bharat A, et al. 2012 update of the 2008 American college of rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken) 2012; 64(5):625-39.
14. Hill J, Bird HA, Lawton C, et al. An evaluation of the effectiveness, safety and acceptability of a nurse practitioner in a rheumatology outpatient clinic. Br J Rheumatol. 1994; 33(3):283-8.
15. Repping-Wuts H, Hewlett S, van Riel P, et al. Fatigue in patients with rheumatoid arthritis: British and Dutch nurses' knowledge, attitudes and management. J Adv Nurs 2009; 65(4):901-11.
16. Sinclair VG, Wallston KA, Dwyer KA, et al. Effects of a cognitive-behavioral intervention for women with rheumatoid arthritis. Res Nurs Health 1998; 21(4):315-26.
17. Koksvik HS, Hagen KB, Rodevand E, et al. Patient satisfaction with nursing consultations in a rheumatology outpatient clinic: a 21-month randomised contolled tiral in patients with inflammatory arthritides. Ann Rheum Dis 2013; 72(6):836-43.
18. Golin CE, Liu H, Hays RD, et al. A prospective study of predictors of adherence to combination antiretroviral medication. J Gen Intern Med 2002; 17(10):756-65.
19. Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care 1989; 27(3 Suppl): S110-27.
20. van Assen S, Agmon-Levin N, Elkayam O, et al. EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis 2011; 70(3):414-22.
21. Luqmani R, Hennell S, Estrach C, et al. The British Society For Rheumatology And British Health Professionals In Rheumatology Standards, Guidelines and Audit Working Group: British Society for Rheumatology and British Health Professionals in Rheumatology Guideline for the Management of Rheumatoid Arthritis (the first two years). Rheumatology (Oxford) 2006; 45(9):1167-9.
22. Grahame R, West J. The Role of the Rheumatology Nurse Practitioner in Primary Care: An Experiment in the Further Education of the Practice Nurse. Br J Rheumatol 1996; 35(6):581-8.
23. Hill J, Bird H, Johnson S. Effect of patient education on adherence to drug treatment for rheumatoid arthritis: a randomized controlled trial. Ann Rheum Dis 2001; 60(9):869-75.
24. Clarke AE, Zowall H, Levinton C, et al. Direct and indirect medical costs incurred by Canadian patients with rheumatoid arthritis: a 12 year study. J Rheumatol 1997; 24(6):1051-60.
25. Lorig K, Holman HR. Long-term outcomes of an arthritis self-management study: effects of reinforcement efforts. Soc Sci Med 1989; 29(2):221-4.
26. Power JD, Perruccio AV, Desmeules M, et al. Ambulatory physician care for musculoskeletal disorders in Canada. J Rheumatol 2006; 33(1):133-9.
Muxin Sun, MD
Faculty of Medicine,
University of British Columbia
Vancouver, British Columbia
Shahin Jamal, MD, FRCPC, MSc
Clinical Assistant Professor,
Division of Rheumatology,
Faculty of Medicine,
University of British Columbia
Vancouver, British Columbia
Jason Kur, MD, FRCPC
Clinical Assistant Professor,
Division of Rheumatology,
Faculty of Medicine,
University of British Columbia
Director,
Arthritis Health Centre
President of BC Society of Rheumatologists
Vancouver, British Columbia |



